Our North East London (NEL) Integrated Care System (ICS) is a partnership that brings together organisations such as local authorities, NHS providers, community and the voluntary sector. Recent guidance has emphasised the importance of partner organisations in having both a population health outlook alongside population health management capabilities in supporting ambitions toward improved health and care outcomes and reduced health inequalities (Model-ICB-Blueprint, NHS Operational Planning Guidance).
What is Population Health?
Population Health is all about improving the health and wellbeing of everyone in our community. It means looking at the bigger picture—not just treating illness, but also understanding and addressing the things that affect our health, like housing, education, income, and lifestyle.
What is Population Health Management (PHM)?
PHM is a way of working within a cycle that helps health and care services plan better and act earlier. Instead of waiting until people get sick, PHM uses information and insights to understand what people need and how we can help them stay well. It’s about being proactive, not reactive.
For example, if data shows that people in a certain area are more likely to develop diabetes, local services can work together to offer support—like healthy eating advice, exercise groups, or mental health support—before problems arise.
Why does this matter to you?
PHM helps make sure that care is tailored to the needs of different groups in our community. Whether it’s older adults needing help to stay independent, families living in poor housing, or communities facing language barriers, PHM helps us understand and respond to these challenges.
In North East London PHM is already making a difference. Local teams are using data to identify local population groups who might be at risk and offering support before health problems become serious. The ambitions are to embed PHM approaches into how organisations and teams work.
The below table indicates some of the beneficial differences that we hope PHM can contribute towards:
| Current Reality | Future with PHM |
| Fragmented view: Clinicians see only pieces of a patient’s journey, creating blind spots and duplication | Holistic understanding: A complete picture of patient needs across health, social care, and wider determinants |
| Reactive firefighting: Health and care teams often respond to crises after they emerge, with limited ability to prevent deterioration | Proactive intervention: Early identification of rising risk enables timely support before crises develop |
| Service-centred design: Patients navigate complex pathways designed around organisational boundaries | Person-centred care: Services wrapped around individuals and communities based on their needs |
| Decision blindness: Limited visibility of population-level patterns means missed opportunities for prevention | Data-informed Decisions: Clear insights into community needs drive resource allocation and service design |
| Professional isolation: Practitioners work within their organisational silos with limited collaboration | Genuine partnership: Cross-system teams collaborating and working together with shared goals and accountability |
| Capacity pressure: High demand and limited resources create constant strain on frontline teams | Sustainable workload: More appropriate interventions and reduced duplication create headroom for care |
| Inequality blind spot: Limited understanding of how interventions impact different community groups | Equity-focused approach: Clear visibility of health and care outcome variations that drive targeted action to reduce inequalities |
Population Health Management – Pathfinder for Analysts – Unlocking linked data for PH – 19 Nov 25
RECORDING
Population Health Management – How to Use Pathfinder – 12 Nov 25
RECORDING
Population Health Management PHM Cycle Webinar – 20 Aug 25
RECORDING
Across the North East London integrated care system (ICS) many stakeholders contribute to the health and wellbeing of our population. The below table provides a high level overview of how PHM could contribute to each audience group:
| North East London Audience Categories |
Key Stakeholder Roles | Key Outcomes or Responsibilities of Group | Key Outputs of Group |
| Strategic Leadership | • Executive Directors • ICB Board Members • Place-Based Directors • Provider Collaborative Leads • Finance Directors |
• Setting strategic vision/direction • Foster Collaboration/ Integration/ Co-production • Resource allocation & Capacity building • System governance • Partnership development • Support cultural shift needed – reactive to proactive • Accountability for outcomes |
• Strategic alignment with National guidance on PHM • Promote system-wide benefits and ROI of PHM • Reducing health inequalities at system level • Resource optimisation • Integration opportunities • Using learning to inform resource allocation |
| Operational Teams | • Commissioning Managers • Population Health Managers • QI Leads • Information Governance Leads • Programme Managers |
• Implementation planning • Operational delivery • Performance management • Risk management • IG compliance and data sharing |
• Operational implementation guidance • Supporting ‘new ways of working’ • Performance metrics and outcomes • Understand PHM cycle methodology • Application of practical tools and resources • Evaluation approaches |
| Clinical and care teams | • GPs • PCN Clinical Directors • INT Leads • Hospital Consultants • Clinical Network Chairs • Directors of Public Health • Nursing Leads • PCN and Practice leadership/ managers |
• Direct patient care • Clinical pathway development • Population health interventions • Clinical leadership • Health promotion and prevention |
• Clinical benefits and improved patient outcomes • Develop ‘new ways of working’ – integration • Patient-centred insights • Practical PHM applications in clinical settings • Evidence-based interventions • How learning cycles improve patient care • Reducing unwarranted clinical variation |
| Technical and analytical teams | • Data Analysts • Business Intelligence Managers • Data Scientists • Performance Analysts • Digital Teams |
• Data analysis and insights • Developing dashboards • Predictive modelling • Supporting evaluation • Technical infrastructure • Data quality |
• Data standards and methodology • Analytics capabilities and tools • PHM Segmentation approaches • Integration of data sources • Technical specifications • Evaluation metrics and measurement |
| Community and partnership | • Patient Representatives • VCFSE Leaders • Community Group Coordinators • Local Authority Partners |
• Community engagement • Patient advocacy • Service user feedback • Community asset development • Local partnership working |
• Engaged local communities • Utilisation/ understanding of PHM approaches • Increased integration and co-production across partners • Addressing health inequalities • How community insights informs learning |
| Cross-system teams | • Wider ICS Staff • Non-PHM Specialists • Supporting Service Teams • Administrative Staff |
• Supporting PHM implementation • Promoting wider adoption • Cross-system working • Administrative support |
• Understand PHM relevance to ICS roles • How PHM connects to new ways of working (integration) • Recognise system-wide benefits of PHM • General awareness and engagement (cultural shif – from reactive to proactive) |
How Does It Work?
PHM aims to bring together the NHS, local councils, voluntary services, housing services, charities, and community groups. Allowing them to share information and work together towards a common objective or health and care outcome for a targeted population group. Sharing data and working collaboratively will help:
- Spot health issues early
- Offer the right support at the right time
- Reduce pressure on hospitals and GPs
- Make better use of public resources
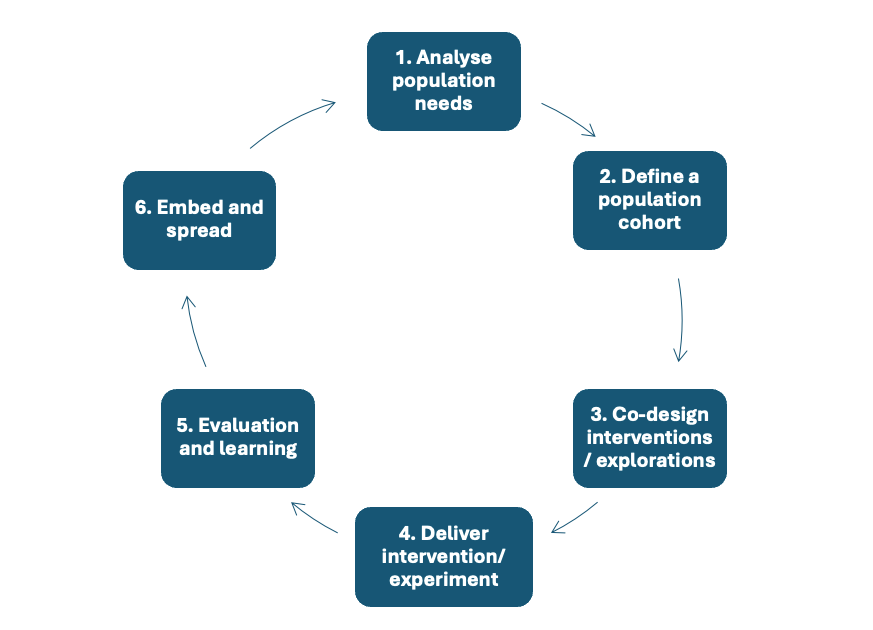
PHM can be viewed as an improvement cycle, and part of what we are aiming to do is promote the understanding and utilisations of PHM across the North East London system partnership organisations:
PHM Improvement Cycle
What’s Next?
There are several elements that together help support the ability of system partners to deliver health and care improvement using a PHM approach. Building upon NEL’s history of collaboration the ambition is to develop these enabling elements, increase the awareness of PHM and how it can be used to improve resident’s health and care outcomes and reduce health inequalities.
As these PHM infrastructures and capabilities mature across North East London, you’ll see more joined-up services, more community support, and more opportunities to take control of your health. Whether it’s through your GP, a local health coach, or a community group, PHM aims to help residents live a healthier, happier life.
Wider Tools and Resources
[1] NHS England » Population health management
This webpage provides an overview of PHM from NHS England. Providing further details on the tools and approaches that can be used to support PHM data driven planning and delivery of care e.g. segmentation, stratification at different the different tiers i.e. system tier, place tier and neighbourhood tier.
[2] NHS England – Population Health Management – Flatpack
Further in-depth detail of PHM including wider context (Quintuple aim) and the three enabler elements for PHM – infrastructure, intelligence, interventions.
[3] Integrated care in action – population health management
The aim of this webpage is to provide an understanding of how integrated care systems are using PHM to improve health and wellbeing via national case study examples.
Supported by NHS England this site provides an introduction to the underlying concepts, data and analysis required to understand and improve a population’s health and wellbeing.
[5] Population Health Academy – Access request (Futures – Futures)
Supported by NHS England the ‘Futures’ platform hosts a Population Health Academy where a multitude of resources, training and networking can be found on PHM. Resources include webinars e.g. ‘PHM for integrated neighbourhoods’, and many case studies to support understanding PHM in practice.
For further information regarding PHM in NEL:
Email: nelondonicb.phm.nel@nhs.net
